By: Laura Horwitz, CSUN Dietetic Intern Cohort 2020-2021

Why does our body need calcium? Along with sodium, chloride and bicarbonate, calcium is one of the major electrolyte minerals1. It is the most prevalent mineral found in the body and is necessary to keep our body functioning.2 Our skeleton stores roughly 99% of the calcium in our body, mostly in our teeth and bones, helping to build and maintain a strong foundation. The remaining 1% is needed for various functions including regulating blood pressure, signaling nerve communication between the brain and other parts of the body, as well as muscle contractions and releasing enzymes and hormones.1,3
Our body cannot make calcium on its own, which is why it is important to eat foods that contain calcium.4 Food sources of calcium include dairy products (e.g., milk, yogurt, and cheese), some seafood (e.g., sardines and salmon canned with bones, oysters and clams), nuts and legumes, and certain vegetables (e.g., leafy greens, turnip, mustard greens, broccoli, kale, collard greens and cauliflower). Some juices (e.g., orange), breads, and cereals have been fortified with calcium.1-5
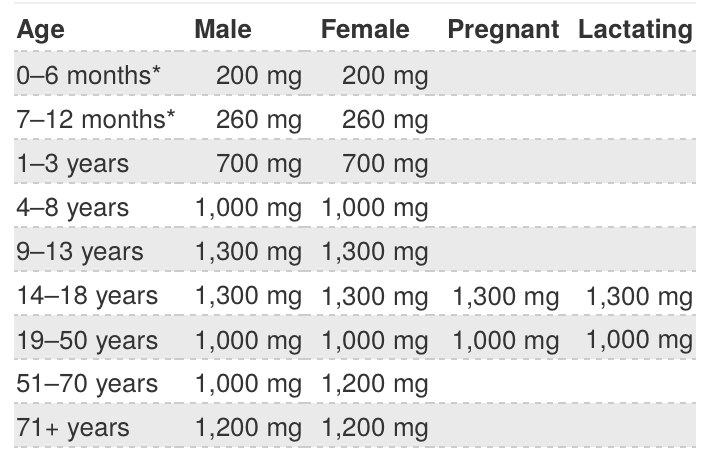
Your daily calcium needs are dependent upon your age and sex.4 A typical dosage per day is 500-100 milligrams (mg).6
Recommended Dietary Allowances (RDAs) for Calcium (Chart from NIH-ODS3)
How can you know if you are getting enough calcium? The International Osteoporosis Foundation’s website has a Calcium Calculator where you can estimate your typical weekly intake: (https://www.osteoporosis.foundation/educational-hub/topic/calcium-calculator).7 Additionally, reading the Nutrition Facts Label on food packaging can tell you the amount of calcium listed by daily value (DV) percentage, based on 1,000 mg per day of calcium (for example: 300 mg of calcium = 30% DV of calcium).4
There are different factors that affect how your body absorbs calcium and how much is absorbed. Newborns, toddlers, and school-age children through their teen years all have a higher rate of absorption than other groups and therefore, have lower calcium requirements (as noted in the recommendations above). Older adults, particularly women with decreased estrogen levels, have a decline in absorption levels due to reduced production of gastric (i.e., stomach and intestinal) juices, which aid in digestion.2
Furthermore, increased intake of calcium lowers the efficacy of its absorption. Diet positively and negatively influences how much calcium is retained in your body. Vitamin D, which is also known for strengthening bones, and protein improve calcium absorption. Sodium, caffeine and alcohol consumption inhibits absorption, as well as foods with oxalic acid (e.g., spinach, sweet potatoes, beans and rhubarb) and phytic acid (e.g., wheat bran, soy isolates, beans and whole grains with high fiber). Calcium elimination via sweat, urine or feces is also affected by sodium, caffeine and alcohol.2,3
Those who may not be consuming sufficient daily amounts of calcium from their diets may have their doctors suggest adding a calcium supplement, which is available over the counter without a prescription. Supplements are best absorbed if taken with food in small amounts spread out during the day.4 The two most common calcium supplements are calcium carbonate, which can cause gas and constipation problems with food digestion, and calcium citrate, which is better tolerated and recommended for older adults and people with absorption illnesses.5 Toxicity can occur if supplements are used by someone that is getting enough calcium from their diet; this can lead to hypercalciuria (high calcium in the urine) and hypercalcemia (i.e., high calcium in the blood), kidney stones and cardiovascular problems.2 Conversely, calcium deficiency can result in hypocalcemia (i.e., low calcium in the blood), renal problems and osteopenia leading to osteoporosis, risking brittle bones or causing an increase of bone fractures.3 Calcium supplements can interact with some medications and cause the absorption rates of both the supplement and the medication to decrease.3 When prescribed a new medication, always discuss with your physician what supplements you are taking.
The U.S. Department of Agriculture and U.S. Department of Health and Human Services released the Dietary Guidelines for Americans, 2020-2025 (9th edition) in December 2020 to provide recommendations on preventing chronic diseases by means of promoting a healthy lifestyle and giving dietary advice on how to meet nutrient needs through the foods we eat and drink.
Crustless Quiche Recipe
Serves 4
Ingredients:
8 oz. 100% Liquid Egg Whites
10 oz. Broccoli florets, frozen, chopped
8 oz. Spinach leaves, frozen, chopped
10 oz. Kale, frozen, chopped
5 oz. Collard greens, frozen, chopped
2 oz. Low sodium cheddar cheese, shredded
2 oz. Low sodium mozzarella cheese, shredded
Directions:
- Mix frozen vegetables together (vegetables can be slightly defrosted)
- Add cheeses and thoroughly mix
- Add liquid egg whites
- Place in 1.5 qt. microwave-safe dish
- Cook in the microwave for 15-18 minutes or until the cheese is melted into the vegetable mix
Nutrition Facts Per Serving:
Calories: 210; Total Fat: 8g; Saturated Fat: 4.5g; Trans Fat: 0g; Cholesterol: 20mg; Sodium: 230mg; Carbohydrates: 12g; Dietary Fiber: 5g; Total Sugars: 3g; Includes 0g Added Sugars; Protein: 19g; Vitamin D: 0mcg; Calcium: 458mg; Iron: 2mg; Potassium: 447mg
NOTE: This dish can be prepared with 2 eggs instead of liquid egg whites, alternative cheeses and alternate vegetables, all of which would change the nutrition facts.
References:
- Raymond JL, Morrow K. Calcium. In: Krause and Mahan’s Food & the Nutrition Care Process. 15th ed. St. Louis, MO: Elsevier; 2021:33-34.
- Gropper SS, Smith JL, Carr, TP. Calcium. In: Advanced Nutrition and Human Metabolism. 7th ed. Boston, MA: Cengage Learning; 2018:426-439.
- U. S. Department of Health & Human Services. National Institutes of Health. Office of Dietary Supplements. Calcium:Fact sheet for health professionals. Website. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/. Accessed January 10, 2021.
- National Osteoporosis Foundation. Calcium and Vitamin D. Website. https://www.nof.org/patients/treatment/calciumvitamin-d/. Accessed January 10, 2021.
- Raymond JL, Morrow K. Calcium. In: Krause and Mahan’s Food & the Nutrition Care Process. 15th ed. St. Louis, MO: Elsevier; 2021:1116-1118.
- Raymond JL, Morrow K. Calcium. In: Krause and Mahan’s Food & the Nutrition Care Process. 15th ed. St. Louis, MO: Elsevier; 2021:199.
- International Osteoporosis Foundation. Calcium. Website. https://www.osteoporosis.foundation/educational-hub/topic/calcium-calculator. Accessed January 11, 2021.
